Validity and Intra Rater Reliability of a New Device for Tongue Force Measurement.
DOI:
https://doi.org/10.9781/ijimai.2022.02.001Keywords:
Device, Temporomandibular Disorders, Tongue ForceAbstract
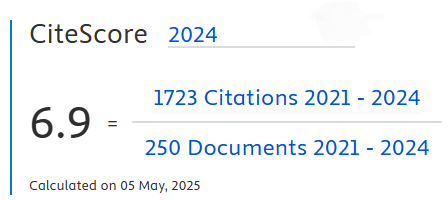
Background. The tongue is made up of multiple muscles both extrinsic and intrinsic. The hyoid, jaw and maxillary complex contain the tongue, which hangs between these structures forming an important biomechanical system. This organ has to work in coordination with craniofacial structures to ensure normal orofacial functioning. There are different devices on the market for tongue force measurement. However, they are not accessible for patients due to their size and very high prices. Likewise, other devices have not yet carried out validity and reliability studies. The purpose of this study was to validate a new device proving that it is accurate compared to the algometer. Moreover, the study wanted to determine the intra-rater reliability of a protocol to assess the maximum tongue force in asymptomatic subjects. Material and methods. This is an observational-longitudinal study with repeated measurements. A prototype device was developed specifically for this study to measure tongue force through force-sensitive resistor sensors. The prototype system was equipped with a device to perform and transmit the measurement and a C++ programming software in the computer to take data from the session. Different formulas were made to calibrate the system. For validity, the force measured by the prototype and the algometer was compared. For intra-rater reliability, 29 asymptomatic Spanish subjects were recruited, and a standardized protocol was carried out for the tests. Results. Experiments to assess validity showed a strong correlation (r>0.97) and an excellent reliability (ICC>0.90) between devices.On the other hand, the intra-rater reliability analysis showed an excellent ICC (0.93) with a 95% CI of 0.86 to 0.97 and a MDC90 of 6.26N. Conclusion. We demonstrated good validity values and high intra-rater reliability for the prototype device for the maximum tongue force.
Downloads
References
W. Wang, C. Di, S. Mona, L. Wang, and M. Hans, “Tongue Function: An Underrecognized Component in the Treatment of Obstructive Sleep Apnea with Mandibular Repositioning Appliance,” Canadian Respiratory Journal, vol. 2018, pp. 1–7, Nov. 2018, doi: 10.1155/2018/2157974.
G. Messina, “The Tongue, Mandible, Hyoid System,” European journal of translational myology, vol. 27, no. 1, p. 6363, Feb. 2017, doi: https://dx.doi.org/10.4081/ejtm.2017.6363
R. White, S. M. Cotton, J. Hind, J. Robbins, and A. Perry, “A Comparison of the Reliability and Stability of Oro-lingual Swallowing Pressures in Patients with Head and Neck Cancer and Healthy Adults,” Dysphagia, vol. 24, no. 2, pp. 137–144, Jun. 2009, doi: 10.1007/s00455-008-9181-0.
H. Yamanashi et al., “Validity of maximum isometric tongue pressure as a screening test for physical frailty: Cross-sectional study of Japanese community-dwelling older adults,” Geriatrics & Gerontology International, vol. 18, no. 2, pp. 240–249, Feb. 2018, doi: 10.1111/ggi.13166.
M. A. Nicosia et al., “Age Effects on the Temporal Evolution of Isometric and Swallowing Pressure,” The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, vol. 55, no. 11, pp. M634–M640, Nov. 2000, doi: 10.1093/gerona/55.11.M634.
H. Taniguchi et al., “Fluoroscopic Evaluation of Tongue and Jaw Movements During Mastication in Healthy Humans,” Dysphagia, vol. 28, no. 3, pp. 419–427, Sep. 2013, doi: 10.1007/s00455-013-9453-1.
J. Kieser, M. Farland, H. Jack, M. Farella, Y. Wang, and O. Rohrle, “The role of oral soft tissues in swallowing function: what can tongue pressure tell us?,” Australian Dental Journal, vol. 59, pp. 155–161, Jun. 2014, doi: 10.1111/adj.12103.
M. Peladeau-Pigeon and C. M. Steele, “Age-Related Variability in Tongue Pressure Patterns for Maximum Isometric and Saliva Swallowing Tasks,” Journal of Speech, Language, and Hearing Research, vol. 60, no. 11, pp. 3177–3184, Nov. 2017, doi: 10.1044/2017_JSLHR-S-16-0356.
J. Furuya, S. Nakamura, T. Ono, and T. Suzuki, “Tongue pressure production while swallowing water and pudding and during dry swallow using a sensor sheet system,” Journal of Oral Rehabilitation, vol. 39, no. 9, pp. 684–691, Sep. 2012, doi: 10.1111/j.1365-2842.2012.02319.x.
P. Bourdiol, A. Mishellany-Dutour, M.-A. Peyron, and A. Woda, “Tonguemandible coupling movements during saliva swallowing,” Journal of Oral Rehabilitation, vol. 41, no. 3, pp. 199–205, Mar. 2014, doi: 10.1111/joor.12135.
K. Hori et al., “Role of tongue pressure production in oropharyngeal swallow biomechanics,” Physiological Reports, vol. 1, no. 6, p. e00167, Nov. 2013, doi: 10.1002/phy2.167.
R. R. Rosa, M. da R. S. Bueno, R. R. Migliorucci, A. G. Brasolotto, K. F. Genaro, and G. Berretin-Felix, “Tongue function and swallowing in individuals with temporomandibular disorders,” Journal of Applied Oral Science, vol. 28, 2020, doi: 10.1590/1678-7757-2019-0355.
M. Corsalini, D. Di Venere, F. Pettini, D. Lauritano, and M. Petruzzi, “Temporomandibular Disorders in Burning Mouth Syndrome Patients: An Observational Study,” International Journal of Medical Sciences, vol. 10, no. 12, pp. 1784–1789, 2013, doi: 10.7150/ijms.6327.
S. N. Robinovitch, C. Hershler, and D. P. Romilly, “A tongue force measurement system for the assessment of oral-phase swallowing disorders,” Archives of physical medicine and rehabilitation, vol. 72, no. 1, pp. 38–42, Jan. 1991.
K. Frändin et al., “Long-Term Effects of Individually Tailored Physical Training and Activity on Physical Function, Well-Being and Cognition in Scandinavian Nursing Home Residents: A Randomized Controlled Trial,” Gerontology, vol. 62, no. 6, pp. 571–580, 2016, doi: 10.1159/000443611.
V. Adams, B. Mathisen, S. Baines, C. Lazarus, and R. Callister, “Reliability of Measurements of Tongue and Hand Strength and Endurance Using the Iowa Oral Performance Instrument with Healthy Adults,” Dysphagia, vol. 29, no. 1, pp. 83–95, Feb. 2014, doi: 10.1007/s00455-013-9486-5.
V. Adams, B. Mathisen, S. Baines, C. Lazarus, and R. Callister, “A Systematic Review and Meta-analysis of Measurements of Tongue and Hand Strength and Endurance Using the Iowa Oral Performance Instrument (IOPI),” Dysphagia, vol. 28, no. 3, pp. 350–369, Sep. 2013, doi: 10.1007/s00455-013-9451-3.
M. Yoshikawa, M. Yoshida, K. Tsuga, Y. Akagawa, and M. E. Groher, “Comparison of three types of tongue pressure measurement devices,” Dysphagia, vol. 26, no. 3, pp. 232–7, Sep. 2011, doi: 10.1007/s00455-010-9291-3.
“IOPI Medical LLC. Iowa Oral Performance Instrument: users manual,” 2008.
State-of-the-Art Pointing Solutions for the OEM, “Force Sensing Resistor Integration Guide and Evaluation Parts Catalog,” Interlinks Electronics, 2002.
“FSRTM Integration Guide Interlink Electronics FSR TM Force Sensing Resistors TM FSR® Integration Guide.”
S. Parmar, I. Khodasevych, and O. Troynikov, “Evaluation of Flexible Force Sensors for Pressure Monitoring in Treatment of Chronic Venous Disorders,” Sensors, vol. 17, no. 8, p. 1923, Aug. 2017, doi: 10.3390/s17081923.
Y. Utanohara, R. Hayashi, M. Yoshikawa, M. Yoshida, K. Tsuga, and Y. Akagawa, “Standard Values of Maximum Tongue Pressure Taken Using Newly Developed Disposable Tongue Pressure Measurement Device,” Dysphagia, vol. 23, no. 3, pp. 286–290, Sep. 2008, doi: 10.1007/s00455-007-9142-z.
J. Kottner et al., “Guidelines for Reporting Reliability and Agreement Studies (GRRAS) Were Proposed,” Journal of clinical epidemiology, vol. 64, no. 1, 2011, doi: 10.1016/J.JCLINEPI.2010.03.002.
T. Ahmed, N. A. Rahman, and M. K. Alam, “Validation and reliability of a prototype orthodontic bracket debonding device equipped with force-sensitive resistor (FSR): a novel method of measuring orthodontic bracket debonding force in vivo,” Prog Orthod, vol. 20, no. 1, p. 26, 2019, doi: 10.1186/s40510-019-0277-x.
M. J. Hjermstad et al., “Studies comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for assessment of pain intensity in adults: a systematic literature review,” Journal of pain and symptom management, vol. 41, no. 6, pp. 1073–93, Jun. 2011, doi: 10.1016/j.jpainsymman.2010.08.016.
S. D. Walter, M. Eliasziw, and A. Donner, “Sample size and optimal designs for reliability studies,” Statistics in Medicine, vol. 17, no. 1, pp. 101–110, Jan. 1998, doi: 10.1002/(sici)1097-0258(19980115)17:13.0.co;2-e.
M. Adam Bujang and N. Baharum, “A simplified guide to determination of sample size requirements for estimating the value of intraclass correlation coefficient: a review,” Archives of Orofacial Sciences, vol. 12, no. 1, pp. 1–11, 2017.
D. E. Hinkle, W. Wiersma, and S. G. Jurs, Applied statistics for the behavioral sciences. Des Moines, Iowa: Houghton Mifflin, 1988.
J. P. Weir, “Quantifying Test-Retest Reliability Using the Intraclass Correlation Coefficient and the SEM,” The Journal of Strength and Conditioning Research, vol. 19, no. 1, p. 231, Feb. 2005, doi: 10.1519/15184.1.
C. Bunce, “Correlation, Agreement, and Bland–Altman Analysis: Statistical Analysis of Method Comparison Studies,” American Journal of Ophthalmology, vol. 148, no. 1, pp. 4–6, Jul. 2009, doi: 10.1016/j.ajo.2008.09.032.
J. M. Bland and D. G. Altman, “Comparing methods of measurement: why plotting difference against standard method is misleading,” Lancet (London, England), vol. 346, no. 8982, pp. 1085–7, Oct. 1995, doi: 10.1016/ s0140-6736(95)91748-9.
S. M. Haley and M. A. Fragala-Pinkham, “Interpreting Change Scores of Tests and Measures Used in Physical Therapy,” Physical Therapy, vol. 86, no. 5, pp. 735–743, May 2006, doi: 10.1093/ptj/86.5.735.
K. W. Wyrwich, “Minimal Important Difference Thresholds and the Standard Error of Measurement: Is There a Connection?,” Journal of Biopharmaceutical Statistics, vol. 14, no. 1, pp. 97–110, Dec. 2004, doi: 10.1081/BIP-120028508.
E. Versi, “‘Gold standard’ is an appropriate term,” BMJ: British Medical Journal, vol. 305, no. 6846, p. 187, 1992, doi: 10.1136/BMJ.305.6846.187-B.
V. S. McKenna, B. Zhang, M. B. Haines, and L. N. Kelchner, “A Systematic Review of Isometric Lingual Strength-Training Programs in Adults With and Without Dysphagia,” American Journal of Speech-Language Pathology, vol. 26, no. 2, pp. 524–539, May 2017, doi: 10.1044/2016_AJSLP-15-0051.
N. P. Solomon, H. M. Clark, M. J. Makashay, and L. A. Newman, “Assessment of orofacial strength in patients with dysarthria,” Journal of Medical Speech-Language Pathology, vol. 16, no. 4, pp. 251–258, 2008.
J. Ulrich Sommer, R. Birk, K. Hörmann, and B. A. Stuck, “Evaluation of the maximum isometric tongue force of healthy volunteers,” European Archives of Oto-Rhino-Laryngology, vol. 271, no. 11, pp. 3077–3084, Nov. 2014, doi: 10.1007/s00405-014-3103-6.
R. K. Balasubramaniam, S. Babu, M. A. Anil, A. L. Varghese, Z. R. Hussain, and D. F. Dsouza, “Does Tongue Hold Maneuver Affect Respiratory – Swallowing Coordination? Evidence from Healthy Adults,” pp. 68–71, 2019, doi: 10.4103/jnsbm.JNSBM.
C. Fernandes, P. Glantz, S. Svensson, and A. Bergmark, “A Novel Sensor for Bite Force Determinations,” Dental materials: official publication of the Academy of Dental Materials, vol. 19, no. 2, 2003, doi: 10.1016/S0109-5641(02)00020-9.
J. S. Schofield, K. R. Evans, J. S. Hebert, P. D. Marasco, and J. P. Carey, “The effect of biomechanical variables on force sensitive resistor error: Implications for calibration and improved accuracy,” Journal of Biomechanics, vol. 49, no. 5, pp. 786–792, Mar. 2016, doi: 10.1016/j.jbiomech.2016.01.022.
L. Paredes-Madrid, A. Matute, A. F. Cruz-Pacheco, C. A. Parra-Vargas, & Elkin, and I. Gutiérrez-Velásquez, “Experimental characterization, modeling and compensation of hysteresis in force sensing resistors,” Revista DYNA, vol. 85, no. 205, pp. 191–198, 2018, doi: 10.15446/dyna.v85n205.66432.
R. Tarricone, A. Torbica, and M. Drummond, “Challenges in the Assessment of Medical Devices: The MedtecHTA Project,” Health Economics, vol. 26, pp. 5–12, Feb. 2017, doi: 10.1002/hec.3469.
Y. Utanohara, R. Hayashi, M. Yoshikawa, M. Yoshida, K. Tsuga, and Y. Akagawa, “Standard values of maximum tongue pressure taken using newly developed disposable tongue pressure measurement device,” Dysphagia, vol. 23, no. 3, pp. 286–90, Sep. 2008, doi: 10.1007/s00455-007-9142-z.
H. C. Crow and J. A. Ship, “Tongue strength and endurance in different aged individuals,” The journals of gerontology. Series A, Biological sciences and medical sciences, vol. 51, no. 5, pp. M247-50, Sep. 1996, doi: 10.1093/gerona/51a.5.m247.
D. A. Robin, A. Goel, L. B. Somodi, and E. S. Luschei, “Tongue strength and endurance: Relation to highly skilled movements,” Journal of Speech and Hearing Research, vol. 35, no. 6, pp. 1239–1245, 1992, doi: 10.1044/jshr.3506.1239.
R. Hayashi, K. Tsuga, R. Hosokawa, M. Yoshida, Y. Sato, and Y. Akagawa, “A Novel Handy Probe for Tongue Pressure Measurement,” Int J Prosthodont, vol. 15, no. 4, pp. 385–8, 2002.
A. Hewitt et al., “Standardized Instrument for Lingual Pressure Measurement,” Dysphagia, vol. 23, no. 1, pp. 16–25, Mar. 2008, doi: 10.1007/s00455-007-9089-0.
K. Tsuga, M. Maruyama, M. Yoshikawa, M. Yoshida, and Y. Akagawa, “Manometric Evaluation of Oral Function With a Hand-Held Balloon Probe,” Journal of oral rehabilitation, vol. 38, no. 9, 2011, doi: 10.1111/J.1365-2842.2011.02202.X.
S. N. Robinovitch, C. Hershler, and D. Romilly, “A Tongue Force Measurement System for the Assessment of Oral-Phase Swallowing Disorders,” Arch Phys Med Rehabil, vol. 72, no. 1, pp. 38–42, 1991.
M. Stone and A. Lundberg, “Three-dimensional tongue surface shapes of English consonants and vowels,” The Journal of the Acoustical Society of America, vol. 99, no. 6, pp. 3728–37, Jun. 1996, doi: 10.1121/1.414969.
H. Takemoto, “Morphological Analyses of the Human Tongue Musculature for Three-Dimensional Modeling,” Journal of Speech, Language, and Hearing Research, vol. 44, no. 1, pp. 95–107, Feb. 2001, doi: 10.1044/1092-4388(2001/009).
K. M. Hiiemae and J. B. Palmer, “Tongue movements in feeding and speech,” Critical reviews in oral biology and medicine: an official publication of the American Association of Oral Biologists, vol. 14, no. 6, pp. 413–29, 2003, doi: 10.1177/154411130301400604.
Downloads
Published
-
Abstract166
-
PDF12